As the opportunity to safely resume in-person therapy becomes an option, there are many things to keep in mind in addition to safety. We have created a list of suggestions to consider in order to best serve your clients and to also keep everyone safe during Feeding Therapy. As always, please check the State/Governmental recommendations and requirements (ASHA Telehealth Guidelines & AOTA Telehealth Regulations by State) in your geographic area, as well as your Institution’s new Health and Safety policies.
*If you have not yet taken the SOS Approach to Feeding (4 Day) Training Conference, some of the strategies discussed below may not be clear to you. Please consider taking one of our Training Conferences, especially now as they are being offered as Virtual Conferences live-streamed and on-line. You can check our Training Schedule to find a conference that may work for you.
Therapist Health Screen
Therapists treating in a Clinic or Hospital Setting should have their temperature taken upon arrival at their clinical setting every day, and they should sign a document verifying they do not have a known COVID-19 exposure. If a Therapist goes into the Client’s Home, the Therapist should take their temperature in the morning before starting their day. This temperature should be sent to the employer who keeps a record of the temperature, along with the Therapist’s daily statement of no known COVID-19 exposure.
Food Preparation & Supplies
All food preparation should be completed by the child’s Feeding Therapist who is gloved and masked throughout the prep. Prepared foods should be placed in sealable containers or baggies. All food prep areas and utensils/dishes are sanitized in between uses.
The Therapist should create one set of foods for themselves, and one set of foods for the Parent/Child. At the end of the session, any extra food should be thrown away or the family could be given their extra portions of the foods to take home with them.
Alternatively, the Therapist could create a Food Hierarchy with the family before the session (via Zoom, email, etc.), and have the family bring their own set of foods to the Clinic for therapy. The Therapist will also create a similar Food Hierarchy for him/herself to use in the clinical setting. All foods are brought to the session in sealed containers/baggies. The family can take home any extra food that they brought in or throw it away at the end of the session.
If the Therapist is treating the child in the family’s home, a Food Hierarchy should be created with the family before the session. It is recommended that the Therapist prepare and bring his/her own food in sealable containers/baggies and that the family prepares their own foods separately in their home. Both the Therapist and Family should prepare foods and other session materials using gloves and masks if possible before the session starts.
- All paper goods and supplies for the session (paper plates, napkins, cups, forks, spoons, knives, toothpicks, kitchen utensils, bowls, etc.) also need to be packaged by a staff person wearing a mask and gloves (perhaps in a large sealable bag or bin with a lid), or the family would need to bring their own set of supplies. The Therapist and Family will each need their own set of matching materials/kitchen tools.
- It is recommended that paper towels or disposable hand wipes be used rather than washcloths or towels for the handwashing part of the routine.
- Separate dish tubs of soapy water for the Parent/Child and the Therapist are also needed.
- The Family could take home any extra paper goods that were leftover to use for Therapy Meals at home, or the sealed bag/bin of supplies could be saved for that Child to use in their next session in the clinic.
- Any kitchen tools/supplies which are not disposable should be sanitized in a dishwasher after the session.
- If you wish to continue transitioning to blowing bubbles as the first step in the Therapy Meal routine, it is recommended that you purchase enough bubble containers/bottles so that each Child, Parent, and Therapist could have their own personal one to use. These must be labeled and can be stored with the Child/Family’s sealed bin/bag of therapy supplies.
- Alternatively, you could use disposable straws (to be thrown away after use), or large plastic/metal straws that can be sanitized in the dishwasher and have the child blow bubbles in the dish tub of soapy water using the straw.
Family Precautions
The morning that the session is scheduled, the Family should take the temperature of everyone in the home (including other siblings, caregivers, etc. who are not going to be attending therapy), and confirm with the clinic that everyone is presumed to be healthy with no known COVID-19 exposures. If any family member has a temperature, the session should be canceled.
Only one Parent/Caregiver and the Child (no siblings) are allowed into the Clinic for the appointment, and they should be wearing masks initially if possible.
Note: Per CDC Recommendations cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.
The family should wait in the car for the Therapist, who will escort them into the Clinic (they can call/text the therapist or front office staff when they arrive). The Therapist should be wearing a mask or a clear plastic face shield, which is preferred if available, and clear plastic gloves. The Child and Parent’s temperature are taken by the Therapist and recorded either before the family gets out of the car or immediately upon their entry into the Clinic. Additionally, the Parent will sign documentation indicating that the Family has no known COVID-19 exposure AND that members of the household do not work in a setting with a high risk of COVID-19 exposure.
- Parents/Caregivers at high exposure risk due to their jobs/place of employment should be encouraged to remain in Telehealth.
- Families who have immune-compromised family members living in the home with them should be encouraged to remain in Telehealth.
- Pens/clipboards are sanitized after each use, and the thermometer is also wiped clean.
Sensory Preparation
It is not recommended to utilize a large sensory gym space where there are many surfaces that would need to be cleaned between each client. Masks and gloves may be required if the Therapist and Child/Parent will be closer than 6 feet from each other. Sensory Preparation ideas will likely need to be individualized to each child, but might include:
- Utilizing outdoor space when possible (continuing to avoid playground equipment unless it can be cleaned between uses).
- Creating a path using chalk, chalk paint, or spray chalk (on grass) from where you would meet the family near their car and bring into the building. Ideas might include drawing different animals for different animal walks to use, shapes to jump or spin on, a ‘race track’ to follow, etc. If there is more than one entrance into your building, you could create one path for older children and one for younger children. Here are some more ideas from Pinterest for inspiration! The blog by Hands On As We Grow also has some great ideas and suggestions.
- Place floor tape (hard floors), velcro (carpet), vinyl floor markers, or laminated signs/symbols on the floor from the front door to the therapy room to create a walking obstacle course to serve as your sensory preparation. This blog by Your Kids OT has some more ideas and examples of what this could look like.
- Encourage the Child to push a heavy item (a large box filled with heavy materials, a cart with weights in it, etc.) down the hallway – this will need to be cleaned between users and/or you could create a box filled with heavy items for each child and have them decorate their ‘vehicle’ which can be used over and over for that child.
- Consider bringing one or two smaller pieces of equipment into the treatment room with you and doing sensory prep in the room. An example might be playing catch with the Child (Therapist wearing clean, clear gloves) with a small weighted ball while the Child jumps on the trampoline. A target game where the Child throws a weighted ball into a bucket would be an alternative for a very small space.
- For a younger child, you could bring in a large therapy ball and have the parent hold their child on their lap to bounce them. An older child may benefit from bouncing on the therapy ball independently or with support from their parent.
- A smaller child may enjoy being carried or pulled in a piece of lycra from the car to the therapy room. The lycra would need to be washed/sanitized between users and/or belong to only one child (kept in a labeled, sealed bag after cleaning).
- Consider also creating some organizing activities that the Family/Child can do together prior to leaving their house or even while the child is riding in the car on the way to therapy so they are hopefully arriving in a regulated state (e.g. listening to calming music, blowing pinwheels, playing with Theraband, etc).
Work with Food
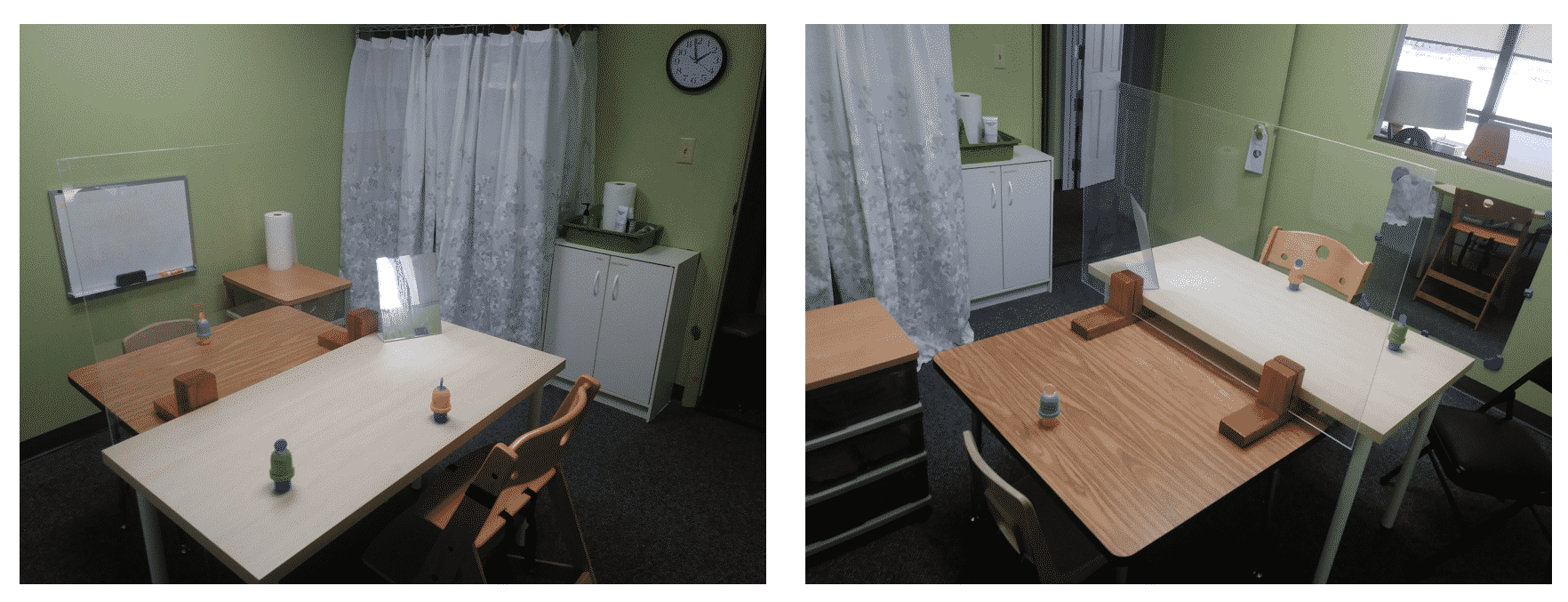
Ideally, the Child will be seen in a large Feeding space at a table that allows the Therapist to be 6 feet away from the Parent and Child (maybe utilizing a long folding table or placing 2 therapy tables together to make one larger table). The Parent and Child would sit at one end of the table with their food and supplies, and the Therapist sits at the other end of the table with his/her foods and supplies. Everyone can remove their masks and gloves at this time since there will be no sharing of materials and there is distance between the Family and Therapist. The Parent presents the bubbles, paper towels/hand wipes, plates, napkins, and foods to the child – one at a time – with the Therapist coaching the Parent as they do this. The Therapist should simultaneously model and complete the actions for themselves from their own set of supplies.
- Everyone should wash/sanitize their hands after removing their mask and before sitting at the table and beginning the work with the food.
 A plexiglass barrier (sometimes called a “sneeze guard”) on the table between the Therapist and Parent/Child may also be an option to consider if you do not have a large enough table or room.
A plexiglass barrier (sometimes called a “sneeze guard”) on the table between the Therapist and Parent/Child may also be an option to consider if you do not have a large enough table or room.- A plexiglass barrier could potentially be acceptable to be used in place of masks during the session, especially if you are spaced out, either using two tables pushed together or one long table to allow for physical distance in addition to the plexiglass barrier.
- If the Therapist is not allowed to go without a mask, Therapists should use a clear plastic face shield type of mask if possible. We have had good success with the type of face shield, which sits on your face like glasses. Talk to your Administrators/Infection Control people about whether this could be an appropriate alternative to a face mask when at the table, especially if you have distance and a plexiglass barrier between yourself and the family. This article from April 2020 supported the use of face masks.
Here is an example of how you might set up your therapy space. You can see in this small room, two tables were pushed together with a plexiglass shield between the table. The therapist sits on one side with one set of supplies and foods, and the parent and child sit on the other side with their own separate set of supplies and foods.
Setting Up for Success
Depending on the skill and experience of the Parent, they can help to lead the session with the Therapist coaching. If the Family is newer to feeding therapy and/or the Parent not as experienced in playing with food, the Therapist will be leading the session from their side of the table with the expectation that the Parent will imitate and model everything the Therapist does.
- It is recommended that a phone or Telehealth meeting with the Parent take place PRIOR to the first Clinic/in-person session so the Therapist can thoroughly explain what will be expected of the Parent in all parts of the session. This is usually easiest if you plan for the Child to be doing something else during this planning time.
- It may be helpful in this meeting to review what types of games the child likes and/or activities that could be used as play themes in the Therapy sessions.
If your clinic has come up with other ideas that have been successful that you wish to share, please contact us and let us know what has been working for you! You can e-mail other suggestions to Lindsay at [email protected].
We hope you continue to stay happy and healthy, safe, and sane during these challenging times!
 ☰ Menu
☰ Menu
 ☰ Menu
☰ Menu
 A plexiglass barrier (sometimes called a “sneeze guard”) on the table between the Therapist and Parent/Child may also be an option to consider if you do not have a large enough table or room.
A plexiglass barrier (sometimes called a “sneeze guard”) on the table between the Therapist and Parent/Child may also be an option to consider if you do not have a large enough table or room.